PÁDRAIG COLLINS AND DAVID FEELY

ABSTRACT
Objectives: To attend to the paucity of research on the profile of presentations cared for by Irish Community Mental Health Teams (CMHTs) by undertaking an audit of the difficulties of service users on the caseload of one CMHT.
Methods: All CMHT members were asked to score each individual on their caseload using a 40-item inventory of common presenting difficulties. These difficulties covered common mental health diagnoses (e.g. depression), common social difficulties (e.g. housing, financial) and common psychological difficulties (e.g. low self-esteem, interpersonal conflict). The needs of 400 of the 601 service users on the team’s caseload are reviewed in this manner.
Results: Of mental health diagnoses, depression and anxiety disorders were most frequently represented. A large percentage of service users (e.g. 41%) presented with distress related to interpersonal conflict. Substance abuse was also highly prevalent (17.5%). High levels of complexity and co-morbidity was noted with 63.5% being scored as having difficulties in three or more domains.
Conclusions: The audit of this CMHT provides data on what presentations are being managed by Irish CMHTs. The audit highlights service implications related to the provision of support for interpersonal and social difficulties and also recommends the development of bespoke care pathways for individuals with high levels of need in multiple domains. Further research in other CMHTs is required to determine the generalisability of these results.
INTRODUCTION
Despite the expenditure of significant resources in the provision of healthcare through community mental health teams (CMHTs) in Ireland we have little to no published data on what presentations are being seen by community teams. In 2017 the predominant disorders evident in inpatient admissions to Irish mental health services were depression (25%), schizophrenia (20%), mania (11%) and alcoholic disorders (7%)1. Inpatient admissions have fallen by over 88% since 1963 representing a transition towards community mental health teams1. This transition has been more recently facilitated by the key policy document ‘A Vision for Change’2 which stressed the need for integrated, community-led, multidisciplinary teams to meet the mental health and wellbeing needs of the Irish population3.
The need for well-resourced and effectively run community mental health care is highlighted by the direct cost of mental health problems in Ireland being estimated at over €3bn4. The proposed role of the CMHT is to provide a comprehensive package of secondary mental health care within a specific geographic area5. However, there is currently a dearth of national data on the prevalence of mental health conditions amongst service users served by these teams. One Irish study compared referrals from primary and secondary care to CMHT psychologists6. It was found that between 36 – 54% of service users were referred for the treatment of a mood disorder, 41 – 46% for an anxiety disorder, up to 12 % for a psychotic disorder, up to 9% for an eating disorder and up to 4% for an impulse control disorder. Of the service users sampled, 26% had at least one comorbid disorder6. This study highlights the diversity and complexity that exists in the caseloads of psychologists working in Irish CMHTs.
A UK study by Greenwood and colleagues (2000) investigated the prevalence rate of disorders in a CMHT in South London serving a population of 1651 service users7. It was found that schizophrenia (28.6%), depression (23.6%), and anxiety disorders (11.1%) were the most common diagnoses. Other UK studies investigated the prevalence rate of personality disorders presenting to CMHTs. It is estimated that between 40 – 52% of service users within these CMHTs suffered from at least one personality disorder8,9. Research has also indicated that up to 44% of CMHT service users had experienced some form difficulties arising from drug and/or alcohol use over the previous year10.
In light of the lack of published data relating to an Irish context, the aim of this current study was to profile the caseload of a CMHT in Ireland in order to determine the prevalence and types of mental health difficulties amongst the service users seen by this team.
METHOD
Setting
A CMHT serving a population of approximately 24,000 people and covering a wide geographical area in Ireland’s midland region was chosen for the purpose of this study. This is largely a rural area, but includes two larger towns. In this area it has been estimated that 1 in 3 referrals to local GPs present with symptoms of psychological distress11. The CMHT was a multidisciplinary team comprised of 1 clinical psychologist, 1 social worker, 3 psychiatrists (1 consultant, 2 NCHD), 2 community mental health nurses, 1 CBT therapist and 1.5 occupational therapists.
Analysts
Each team member was asked to fill in the audit form for each service user for whom they were the keyworker (all service users had one named keyworker, thereby preventing double-scoring) using the guidance outlined below. Consequently the full range of disciplines participated in the audit. The presentations of 400 service users (aged 18+) who were on the CMHT caseload were consecutively analysed. This constituted 66% of the total team caseload (n=601). The presentations of the remaining 201 service users were not analysed due to time constraints on the audit. A randomised sample (n=15, random number generator) of these 201 service users was later analysed and revealed a profile of presentations similar to that of the large sample.
Audit Items
The audit items (36) were based on the topics covered by the large-scale Psychiatric Morbidity survey carried out in the UK (Office of National Statistics12). This study was chosen as a guide as it was the closest published example of a study that covered diagnostic and non-diagnostic mental health categories. On piloting, CMHT clinicians requested an additional 4 items relating to forensic issues which were added. (Full list of items available on request from corresponding author).
Threshold Judgements: The psychiatric morbidity UK survey involved lay interviewers surveying individual members of the public, followed, for a subset, by clinical interviews. For the purpose of this audit, skilled mental health professionals scored individuals on a caseload with which they would be very familiar. The professionals were advised, for diagnostic categories (e.g. depression, personality disorder), to score an item (present/absent) if a formal diagnosis had been previously given. As such team members were not required to make any new diagnostic decisions but simply apply pre-existing diagnoses in relation to formal mental disorders. For non-diagnostic categories e.g. ‘distress arising out of poor financial situation’, the professionals, who were highly experienced mental health practitioners, were advised to score an item as present if it met the DSM V (2013) threshold of clinical significance i.e. “causes clinically significant distress or impairment in social, occupational or other important areas of functioning”13.
International best practice guidelines on ethical approval (i.e. UK National Research Ethics Service29) were consulted indicating that standard internal service audits of this nature did not require additional external ethical approval.
RESULTS
Service Users
The sample of service users included 170 (42.5%) males and 230 (57.5%) females. The age range was 17 – 88 years. The vast majority of the sample was of a White-Irish ethnicity. Detailed information on non-Irish ethnicity was not collected.
Disorder Specific Analysis
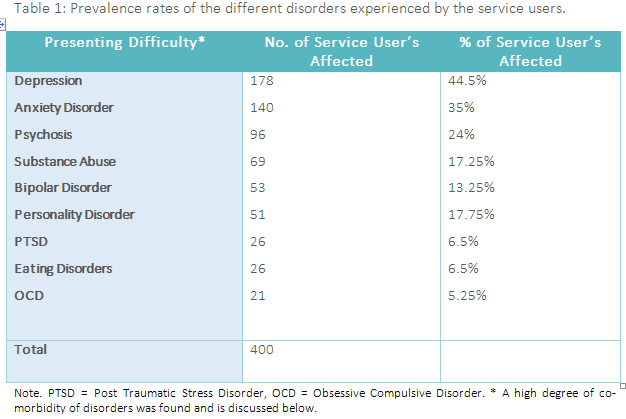
229 service users (57.25%) were rated as having problems associated with depression or anxiety, with 89 (22.25%) individuals rated as having difficulties with both depression and anxiety. 96 people (24%) were rated as experiencing problems associated with psychosis and 69 people (17.25%) with substance abuse. Meanwhile, 53 people (13.25%) were rated as presenting with bipolar depression, 51 people (12.75%) with a personality disorder, 26 (6.5%) with an eating disorder, and 26 (6.5%) with Post Traumatic Stress Disorder (PTSD). Table 1 presents a summary of the prevalence rates for each of the different disorders experienced by the service users sampled.
Interpersonal Difficulties
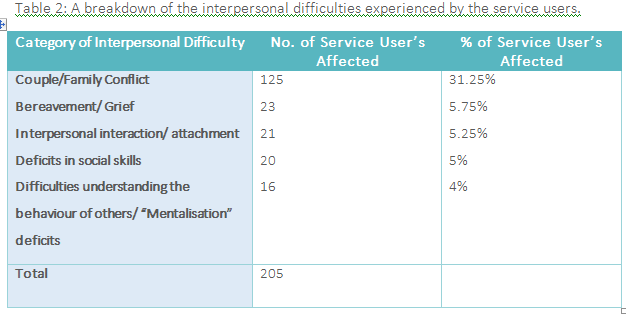
164 service users (41%) were scored as experiencing some category of interpersonal difficulty. This figure is broken down further in Table 2 below.
Social/ Environmental Difficulties
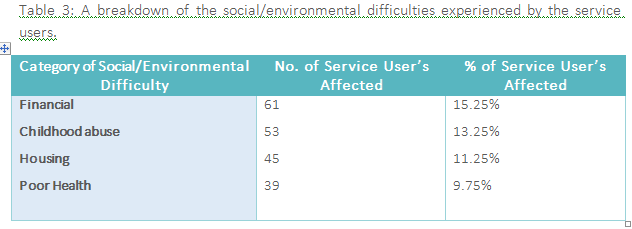
61 individuals (15.25%) were scored as experiencing financial problems, 53 individuals (13.25%) as the victim of childhood abuse, 45 individuals (11.25%) as having problems associated with housing issues, 39 individuals (9.75%) as experiencing poor physical health. These figures are presented in Table 3 below.
Level of Complexity
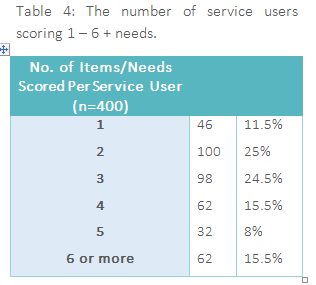
354 (88.5%) scored as having more than one source of mental health distress (e.g. depression and financial difficulties), with 62 service users (15.5%) presenting with 6 or more needs. This information is presented in Table 4 below.
DISCUSSION
We know little from the published research to date on what types of mental health difficulties present to Irish Community Mental Health Teams or the prevalence of specific psychosocial difficulties. Effective resource allocation and utilisation requires some knowledge of the types of difficulties with which CMHTs are faced. This research aimed to attend to this deficit in our knowledge by engaging in an initial audit of one CMHT and examining not only the prevalence of specific mental health disorders but to also look more broadly at the diverse social and psychological difficulties that commonly present at a CMHT.
Diagnostic Prevalence Rates
In keeping with a large body of research regarding the high prevalence of depression14, depression was the most prevalent difficulty scored by team members with 178 (89 with depression alone, 89 with depression and anxiety) out of the 400 (44.5%) sampled service users. Similarly, the recorded high levels of anxiety disorders also mirror international research in this area15.
Somewhat less prevalent than expected are ratings of Personality Disorder (12.5%). This is in keeping with research in prevalence rates in a community sample16 but with a clinical sample one could have expected a higher prevalence. This may be influenced by the continuing stigma associated with the diagnosis of personality disorder and therefore, at times, a potential bias towards using a possibly less stigmatising diagnosis (e.g. depression). It may also reflect inadequate assessment for personality disorder. To address this limitation, recent discourse in mental health has called for a move away from diagnostic categories towards a formulation based framework of understanding people’s distress17.
The rates of PTSD are in keeping with other research with clinical samples but this may itself be an underestimate of its true prevalence (see Zinmmerman & Mattia, 1999, for discussion)18. The rates scored for psychotic symptomatology (24%) are comparable to those found by the Greenwood et al. (2000) UK study for Schizophrenia (28%) with the recording of mood lability/ bipolar disorder symptomatology somewhat higher than the Greenwood sample (13.25% vs. 8.2%), possibly due to additional individuals in the Greenwood sample with significant mood lability being assigned a “schizoaffective” diagnosis (2.9%)7.
Psychosocial difficulties prevalence rates
Of particular interest, due to a dearth of similar research in this area, are the results relating to the types and prevalence of psychosocial difficulties with which individuals present to a CMHT.
It has been long recognised that individuals commonly present with a mental health condition at a time of transition or major stress in their life19, 20. What is striking from this sample is the degree to which interpersonal difficulties may represent the source of such stress with 41% of the sample being scored as experiencing these difficulties. Acknowledging that professionals will be not be aware of such conflict in service users’ lives, this figure may significantly underestimate the prevalence of such difficulties. These results highlight the importance for clinicians to ask about important relationships during assessment. The level of such difficulties may also support the role of therapies with an explicit interpersonal focus e.g. Interpersonal Therapy for Depression21 or Behavioural Family Therapy for Psychosis22.
It is noteworthy that a significant proportion of service users were rated as having a variety of different social difficulties such as housing (11.25%), finance (15.25%) and also that wellbeing issues, such as poor health (9.75%) also prominently feature. These results support the importance of the provision of support to service users around social difficulties. This finding is consistent with research over the last four decades (e.g. from Brown & Harris, 1978 to Murali & Oyebode, 2004)23, 24 highlighting the importance of social difficulties in the aetiology and maintenance of mental health difficulties.
The levels of childhood abuse reported were significant (13.5%) but again, however, may represent a large underestimate cognisant that many such victims do not report to professionals their experience of abuse25. Consequently, further assessment of adverse childhood experiences may also be indicated in future research.
Complexity and co-morbidity
A high level of co-morbidity was noted in particular in relation to depression and anxiety with as large a number of service users being rated as suffering from a combination of these difficulties. It is also noteworthy that across the different diagnostic and psychosocial domains that the vast majority of service users (63.5%) were rated as having difficulties in 3 or more areas. This indicates a level of complexity that justifies the utilisation of a multidisciplinary team service to meet the range of needs and complexity of presentations.
The results also indicate a significant minority of individuals (15.5%) with a high level of need having 5 or more domains scored as areas of need. There may be some utility in teams identifying these cases for specialist review and care coordination. Other jurisdictions have developed “complex cases” teams and/or specialist service (e.g. assertive outreach, rehabilitations and recovery, personality disorder services) as well as bespoke care pathways to attend to the needs of these individuals. This model of resource allocation acknowledges that where these cases are cared for within a generic CMHT model, there is the potential of this minority of presentations to take up a significant proportion of the CMHT resource, and that generic teams or generic care pathways may not always meet the specific needs of these complex presentations. Other case-load weighting models use measures of complexity to allocate fairly across the team the number of highly complex presentations with which each team members may be asked to work, thereby ensuring that service users are not being seen by team members overwhelmed by a caseload of highly complex presentations.
Conversely, the significant minority of service users (36.5%) scoring as having difficulties in only one or two domains may indicate that their remains a large proportion of service users whose needs could potentially be met with a well-developed primary care service. A “stepped-model” approach whereby service users receive the intensity of support required by their difficulties (as distinct from all service users being referred to a generic secondary care mental health team) may provide the best clinical and economic use of limited resources. Certain Primary Care Psychology services (e.g. the Access to Psychological Therapies Ireland service)26 currently provide evidence-based psychological treatments for individuals presenting with conditions such as depression and anxiety on a ‘stepped-care’ basis. There may be a role for primary care practitioners, in partnership with secondary care CMHTs, in guiding GP referrals in this regard.
Care Clusters
The results also potentially indicate that there may be a usefulness in developing “care clusters” either around diagnostic criteria (e.g. “affective disorders”, “bipolar and psychotic disorders” and “personality / complex presentations”) or perhaps more helpfully around the broader biopsychosocial pattern of needs presenting (i.e. by using a clustering tool such as the “Mental Health Clustering Tool”27 which is a further elaboration of the HoNOS; ‘Health of the Nation Outcome Scale’28). Such clustering may allow the development of specific specialist skills and services within a CMHT as bespoke care pathways are developed and clinicians develop specialist interests.
Limitations
The scoring of psychosocial difficulties as ‘present’ or ‘absent’, while facilitating a large scale audit, may belie the complexity of such difficulties which tend to exist along a spectrum. The rural nature of the population may present a profile that differs from that seen in more urban areas. Service users might themselves, if consulted, have defined their difficulties using terms or categories different from those utilised in this audit.
Implications for Service Provision and Future Research
These results indicate the importance of interventions focused on attending to interpersonal and social difficulties, as well as clinical symptomatology. It highlights that a sub-cluster of service users may present with high levels of biopsychosocial need and requires specialist input. It outlines the potential utility of a stepped care model of service provision. Finally, it identifies the need for more comprehensive research on the demands placed on standard CMHTs and the most effective interventions that might be offered by those teams
This study provides some helpful indicative data on the type of presentations attending a particular CMHT. While manualised, structured clinical interviews of each individual service users by trained researchers might provide a more rigorous dataset (and could be a focus of future research) few CMHTs have access to such resources. Nevertheless, it is incumbent upon all health services to audit the difficulties with which they are working to ensure their resources are being used in the best ways possible. This audit represents a first step in this direction and explicitly includes those psychosocial difficulties (e.g. financial problems, interpersonal conflicts) which are central to the work of CMHTs but commonly absent in diagnostic-led audits.
CONCLUSION
An analysis of the presentations to a rural Irish CMHT was undertaken. Members of the multidisciplinary CMHT scored individuals on their caseload using a 40-iterm inventory which outlined common clinical diagnoses, as well as psychological and social difficulties. The results are outlined in detail and their potential implications discussed. Further research could usefully attend to exploring this area further including the use of additional tools such as structured clinical assessments to determine whether these results generalise to other Irish CMHTs (especially those in urban areas). Such data could increasingly inform the practice of CMHTs and ensure that their resources and skills are being best utilised to meet the needs of their communities.
REFERENCES
- Health Research Board HRB Statistics Series 22. Irish Psychiatric Units and Hospitals. Census 2013. NIPRS Team: Daly A, Walsh D, Moran R. HRB Stationery Office, Dublin. 2014.
- Department of Health & Children. ‘A Vision for Change’ Report of the Expert Group on Mental Health Policy. Stationery Office, Dublin. 2006.
- De Búrca S, Armstrong C, Brosnan, P. Community mental health teams determinants of effectiveness in an Irish context. Health Systems Research Centre: Limerick. 2010.
- O’Shea E., Kennelly B. The Economics of Mental Health Care in Ireland. NUIG/Mental Health Commission 2008.
- Collins P., Byrne M. A call to co-ordinate mental health teams. The Irish Psychologist 37(8), 212-6. 2011.
- Curtis L, Byrne M. Comparison of referrals from primary and secondary care to CMHT psychologists. Irish Journal of Psychological Medicine 26(2), 73-75. 2009.
- Greenwood N., Chisholm B., Burns T., Harvey K. Community mental health team case-loads and diagnostic case-mix. Psychiatric Bulletin 24(8), 290-293. 2000.
- Newton-Howes G., Tyrer P., Anagnostakis K., Cooper S., Bowden-Jones O., Weaver T. The prevalence of personality disorder, its comorbidity with mental state disorders, and its clinical significance in community mental health teams. Social psychiatry and psychiatric epidemiology 45(4), 453-460. 2010.
- Keown P., Holloway F., Kuipers E. The prevalence of personality disorders, psychotic disorders and affective disorders amongst the patients seen by a community mental health team in London. Social psychiatry and psychiatric epidemiology 37(5), 225-229. 2002.
- Weaver T., Madden P., Charles V., Stimson G., Renton A., Tyrer P., Barnes T., Bench C., Middleton H., Wright N., Paterson S., Shanahan W., Seivewright N., Ford C. Comorbidity of substance misuse and mental illness in community mental health and substance misuse services. The British Journal of Psychiatry 183(4), 304-313. 2003.
- Hughes M., Byrne M., Synnott J. Prevalence of psychological distress in general practitioner adult attendees. Clinical Psychology Forum 206, 33-38. 2010.
- Singleton, N., Bumpstead, R., O’Brien, M., Lee, A., & Meltzer, H. Psychiatric morbidity among adults living in private households, 2000. International Review of Psychiatry, 15(1-2), 65-73. 2003.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (-5th ed.). 2013.
- World Health Organisation. Mental Health in the WHO European Region. Fact Sheet EURO/03/03. World Health Organisation: Geneva. 2003.
- Kessler R.C., Berglund P.A., Demler O., Jin R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry 62(6), 593-602. 2005.
- Coid J. Epidemiology, public health and the problem of personality disorder. British Journal of Psychiatry 44, 3-10. 2003.
- Boyle, M., & Johnstone, L. Alternatives to psychiatric diagnosis. The Lancet Psychiatry, 1(6), 409-411. 2014
- Zimmerman M, & Mattia J.I. Is posttraumatic stress disorder underdiagnosed in routine clinical settings? The Journal of Nervous and Mental Disease 187, 420–428. 1999.
- Brown G.W., Harris T.O. Petro J. Life events and psychiatric disorders, Part 2: Nature of causal link. Psychological Medicine, 3, 159-176. In: Lukoff D, Synder KS, Ventura J, Nuechterlein KH. (1984) Life events, familial stress and coping in the developmental course of schizophrenia. Schizophrenia Bulletin 10, 258-292. 1973.
- Mundt C., Reck C., Backenstrass M., Kronmuller K., Fiedler, P. Reconfirming the role of life events for the timing of depressive episodes. A two year prospective follow up study. Journal of Affective Disorders 59(1), 23-30. 2000.
- Weissman M.M., Markowitz J.C., Klerman, G.L. Clinician’s quick guide to interpersonal psychotherapy. Oxford University Press: New York. 2007.
- Fadden G. Family Interventions and Psychosis. In Beinart H, Kennedy P, Llewelyn S. (Eds.). Clinical Psychology in Practice. Blackwell Publishing: Oxford. 2009.
- Brown G.W., Harris T.O. Social origins of depression: A study of psychiatric disorders in women. London: Tavistock. In Cohen S, Kessler RC, Gordow LU (Eds), Measuring Stress: A Guide for Health and social scientists, pp. 59-79. Oxford University Press: New York. 1978.
- Murali V., Oyebode F. Poverty, social inequality and mental health. Advances in Psychiatric Treatment 10, 216–224. 2004.
- Cawson P., Wattam C., Brooker S., Kelly G. Child Maltreatment in the United Kingdom: A study of the prevalence of child abuse and neglect. NSPCC: London. 2000.
- Kelly J., Sammon N., Byrne M. APSI: A proposed integrative model for suicide prevention. Irish Journal of Psychological Medicine, 31(3), 203-212. 2014.
- Department of Health, UK. Mental Health Clustering Booklet. 2012. Retrieved from https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216217/dh_132656.pdf
- Wing J.K., Curtis R.H., Beevor A.S. HoNOS: Health of the Nation Outcome Scales: Report on Research and Development July 1993-December 1995. Royal College of Psychiatrists: London. 1996.
- Health Research Authority: NHS ‘Defining Research’ Accessed at https://researchsupport.admin.ox.ac.uk/sites/default/files/researchsupport/documents/media/defining-research.pdf
AUTHORS
Dr. Pádraig Collins, Senior Clinical Psychologist, Roscommon, HSE-West. padraig.collins@hse.ie
Dr David Feely, Clinical Psychologist, HSE-West.